
incentive Spirometer Device: Simple Way to Monitor Lung Capacity
Living with a chronic lung condition can make each breath feel precious—and sometimes, uncertain. Whether you’re managing asthma, caring for a loved one with COPD, or working on the front lines of community health, understanding and monitoring lung function is crucial for safety, confidence, and quality of life. The spirometer—an easy-to-use yet powerful tool—has transformed not only medical care but also everyday self-management for millions. In this post, we’ll demystify the spirometer, highlight its life-changing impact, and offer practical steps you can take today to put the power of knowledge in your (or your loved one’s) hands.

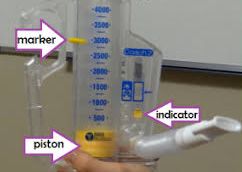
What Is a Spirometer, and Why Does It Matter?
A spirometer measures how much air you can inhale and exhale, and how quickly you can breathe out. This may sound simple, but it’s the foundation of diagnosing and managing conditions such as asthma, chronic obstructive pulmonary disease (COPD), and other respiratory illnesses.
A spirometer is a device that helps patients increase their lung capacity and improve their breathing. It works by providing visual or audible feedback when inhaling and exhaling. This feedback encourages the patient to take deeper breaths and reach their target volume, which helps increase the amount of air they can take in and out of their lungs. This can help reduce the risk of developing respiratory conditions and can also aid in post-operative recovery.
But the spirometer’s magic goes far beyond just numbers. Think of it as a window into your (or your patient’s) lung health, helping answer critical questions:
- Are symptoms under control?
- Is medication working?
- Is it time to adjust your action plan?
For many, having this information at home means fewer unexpected flare-ups and a greater sense of control over daily life.
Real Story: Anaya, a teacher living with asthma, once felt anxious about everyday activities. After learning to monitor her lung function at home with a simple handheld spirometer, she noticed patterns—when her numbers dipped, she could act early, adjust her environment, and talk to her doctor before a crisis developed.  “It’s given me confidence and freedom,” she says.
“It’s given me confidence and freedom,” she says.
Breaking Down Barriers: Common Myths and Practical Tips
Many people hesitate to use a spirometer because they assume it’s complex or only for doctors’ offices. Good news: Times have changed. Today’s models—some smaller than a smartphone—are user-friendly, accurate, and even connect with health apps on mobile devices.
Myth 1: “It’s painful or uncomfortable.”
Reality: Spirometry is safe, simple, and painless. The test only involves breathing into a mouthpiece. Some people may feel slightly dizzy afterward due to deep breathing, but that passes quickly.
Myth 2: “It’s too technical for home use.”
Reality: Most home devices come with clear instructions or step-by-step videos. Some even give instant feedback with color-coded results.
Myth 3: “Spirometry is only for people with asthma.”
Reality: Spirometry is used to diagnose and monitor many conditions — including COPD, chronic bronchitis, emphysema, and even restrictive lung diseases. It’s also helpful in assessing overall lung health, especially for smokers or people exposed to pollutants.
Myth 4: “You only need spirometry if you have symptoms.”
Reality: People at high risk (such as smokers, workers exposed to dust or chemicals, or those with a family history of lung disease) should have periodic spirometry even without symptoms. Early detection can prevent serious damage.
Myth 5: “A normal spirometry result means I don’t have lung disease.”
Reality: Some lung problems — especially early-stage or intermittent conditions — might not show up on a single spirometry test. Additional tests or repeat measurements may be needed for a full picture.
Quick Tips for Getting the Most from Your Spirometer
- Practice Good Technique: Sit upright, form a tight seal around the mouthpiece, and blow out fast and hard.
- Test at Regular Times: Consistency helps track trends—try testing in the morning and evening, or when symptoms arise.
- Keep a Symptom Journal: Jot down readings alongside notes about how you feel and any triggers you notice.
- Share Results: Bring your device or logbook to appointments or use telehealth features to share data electronically.
Before the Spirometer test
Avoid caffeine before the procedure
Ask your healthcare provider which medications you should avoid on the day of the test
Do not smoke within 24 hours of the test
Do not drink alcohol within 4 hours of the test
Do not exercise strenuously within 30 minutes of the test
Wear comfortable clothing that allows one to breathe easily
Do not eat a heavy meal within two hours of the test
How a spirometer is done
During a spirometry test, a patient:
A special mouthpiece will be placed in the patient’s mouth. The device then records and analyzes airflow and volume.
The patient will be asked to seal their lips tightly around the mouthpiece
A clip will be used to block the nose to keep air from leaking out of the nose
The patient will be asked to exhale until the lungs are empty followed by a deep breath to fill up the lungs
The patient will then exhale as forcefully and completely as possible into the mouthpiece connected to the spirometer until the lungs are empty
The test will be repeated three times
Key Measurements
FVC (Forced Vital Capacity): The total amount of air exhaled after a deep breath.
FEV₁ (Forced Expiratory Volume in 1 Second): The amount of air exhaled in the first second — used to assess airway obstruction.
FEV₁/FVC ratio: Helps distinguish between obstructive (e.g., asthma, COPD) and restrictive (e.g., pulmonary fibrosis) lung diseases.
A spirometer is much more than a gadget—it’s a gateway to better health, peace of mind, and proactive living. By embracing this tool, anyone affected by chronic lung issues can transform uncertainty into confidence, and caution into courage. Whether you’re addressing your own health or supporting someone else’s journey, remember: every strong breath is worth celebrating, and every day presents a new opportunity to take charge.
Ready to Take the Next Step? Explore more on spirometry, access guides, or connect with a support group at patientinformationcorner.com. Share your story or tips in our community discussion—your journey might empower someone else to breathe easier today!
Breathe with confidence. We’re here to help—every step, and every breath of the way.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

